COVID-19 has left a profound and lasting impact on global health, but one lesser-known consequence is the significant rise in cardiovascular events—particularly heart attacks—among survivors. Studies now show a compelling link between COVID-19 and a sudden increase in heart attack risk, even months after recovery. This article explores the causes, risks, timelines, and prevention strategies while integrating the latest research and expert opinions.
Understanding the Link Between COVID-19 and Heart Attacks
How COVID-19 Affects the Heart
COVID-19 is primarily known as a respiratory illness, but it has a systemic impact that includes cardiovascular damage. The virus can inflame blood vessels, increase clotting, and elevate stress on the heart.
Post-COVID Heart Attack Risk: The Data
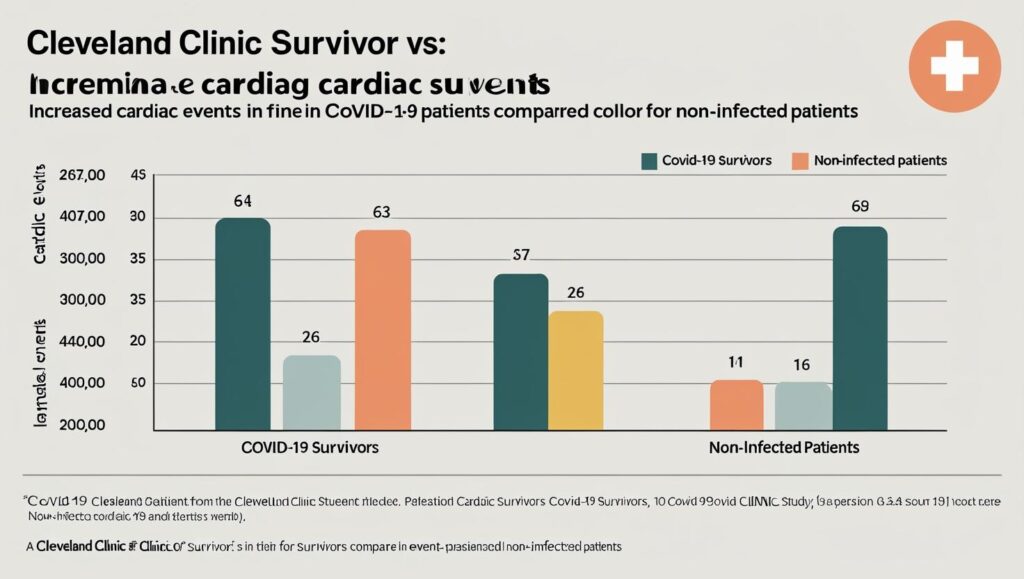
A study published by Nature Medicine found that individuals who had COVID-19 were at 2–4 times greater risk of developing heart attacks up to a year post-infection.
Research from the Cleveland Clinic indicates that even mild cases can lead to elevated risk of cardiovascular events.
The Science Behind the Surge
Long-Term Inflammation and Clotting
One of the core theories behind the increased heart attack risk post-COVID is persistent inflammation and endothelial dysfunction.
COVID-19 can leave blood vessels inflamed, increasing the chances of clot formation.
Long-term inflammation can destabilize plaque in arteries, leading to myocardial infarctions.
ACE-2 Receptor and Cardiac Involvement
SARS-CoV-2 binds to ACE-2 receptors, which are found not only in lungs but also in the heart and vascular system.
Who Is Most at Risk?
High-Risk Populations
Certain demographics have shown to be more vulnerable:
Adults over 50
Those with pre-existing heart disease
People with obesity, hypertension, or diabetes
Unexpected Vulnerability in Younger People
Interestingly, even younger adults without previous cardiovascular issues have reported cardiac events following COVID.
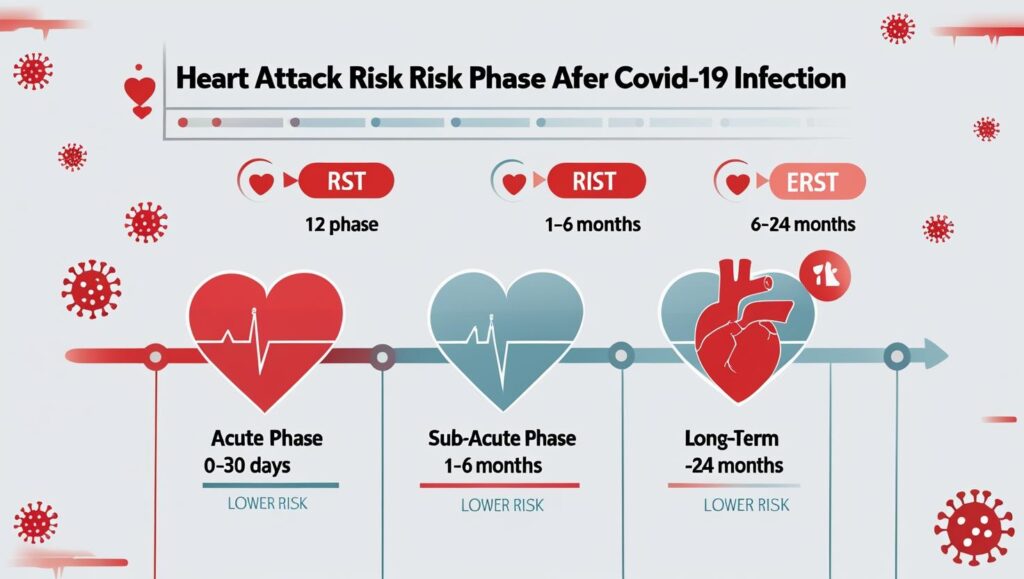
Timeline: When Does the Risk Peak?
Acute Phase (0–30 Days)
Initial risk spike due to active viral load and inflammation.
Sub-Acute Phase (1–6 Months)
Inflammatory markers may still be elevated, making this a critical monitoring period.
Long-Term Phase (6–24 Months)
Risk remains elevated, though begins to taper in most cases.
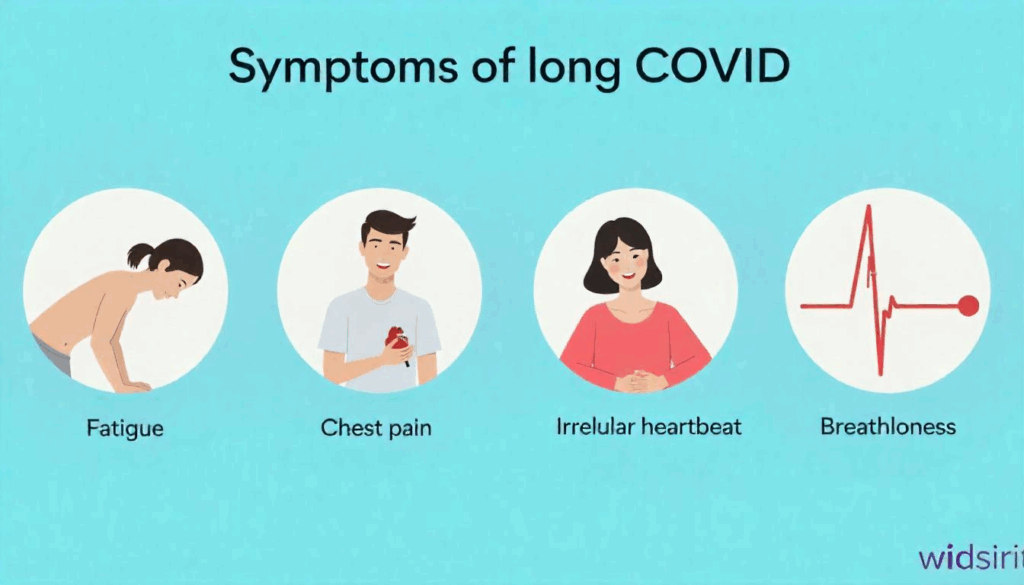
Related Complications: Not Just Heart Attacks
COVID-Related Cardiac Arrest
Cardiac arrest incidents have also risen among COVID survivors.
Other Cardiovascular Issues
Arrhythmias
Myocarditis
Stroke
Prevention and Monitoring

What You Should Do If You Had COVID
COVID
Schedule a heart health check-up
Monitor for symptoms like chest pain, shortness of breath, and palpitations
Maintain a heart-healthy diet
Avoid smoking and manage stress levels
Role of Vaccination
Studies show that vaccinated individuals have a significantly reduced risk of long-term cardiovascular complications.
Latest Research and Case Studies
Cleveland Clinic Study
Found increased risk of cardiac events even in asymptomatic COVID-19 cases.
UK Biobank Analysis
Confirmed long-term elevated risk across all age groups
Addressing Misinformation
Separating Fact from Fiction
The internet is rife with misinformation. Always rely on studies from reputable journals and institutions.
What the Experts Say
Cardiologists advise all COVID-19 survivors—regardless of symptom severity—to remain vigilant and undergo cardiovascular screening.
Conclusion
The post-COVID era has introduced new health challenges, with heart attacks emerging as a serious long-term concern. With growing evidence supporting the link between COVID-19 and elevated heart risks, awareness and proactive care are crucial. Whether you’ve had COVID-19 recently or long ago, understanding your risk and taking preventive measures can make all the difference.